As of Jan. 1, 2019, in the name of transparency and in accordance with ACA, all hospitals must post their list of prices online. But what you find on their sites, that is if you can sort through them to find the list, is a list medical codes, abbreviations, and costs. The list may be in some sort of discernible order and maybe not. The initial roll out will serve to confuse more than illuminate but is a step in the right direction. As I have said before, transparency is needed for the overall reform of healthcare. Unless the payment system is reformed there can be no lasting reform of the system.
Any patient who has ever tried to find out how much a hospital test, procedure or stay will cost prior to getting the test or procedures knows all too well the frustration. “It depends” is a common reply from the billing department and even from insurers. While information is always welcome, the new payment data falls short of providing consumers with usable information unless, of course, you happen to be a medical coder.
The requirement to post charges, which can be a Microsoft Excel spreadsheet, maybe helpful but, get this, currently there is no penalty, i.e. fine, for failing to do so. The master file is called the chargemaster, so you might find it by typing the hospital’s name into your favorite search engine and use the keywords “billing” or “chargemaster.” If you get no results as I have on several hospitals, do not be surprised. I have tried calling the hospital but still no luck yet. (Search chargemaster with the name of the hospital try to locate one.)
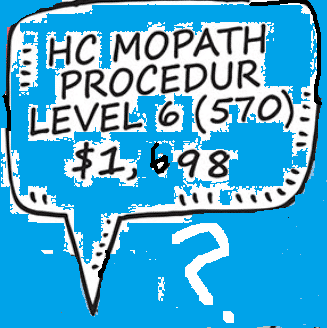
Which services, treatments, drugs or procedures a patient will receive during a hospital stay is often unknowable. And the charge listed is only one component of a patient’s total bill. For example, an MRI of the abdomen has additional costs, such as the charge for the radiologist who reads the exam and that cost is not likely to be found when the radiologist is not employed by the hospital.
Though chargemaster rates are quite different from the lower, negotiated rates that insurers pay, they are the basis for what patients pay who have no insurance or their provider is not in their insurer’s network. Out-of-network patients are often open to “balance bills,” charges for the difference between what their insurer pays for the care and the full charge. The chargemaster is what hospitals would like to be paid, so posting them publicly should make hospitals more accountable for their prices and in turn compete more transparently.
